By Dr Jeff Carroll on February 28, 2016. Edited by Dr Ed Wild
The third and final day of the 2016 Huntington’s Disease Therapeutics Conference brings updates on cell replacement therapies including stem cells; and new ways to assess and model the progression of HD to help understand it and run crucial clinical trials.
Thursday morning – replacing cells, restoring networks
The day in Palm Springs starts with a session on the once-crazy idea that we might be able to replace brain cells.
Ali Brivanlou is a ‘developmental biologist’ – one who studies the process by which a fertilized egg becomes a mature adult. Brivanlou’s lab uses embryonic stem cells to study human development. These ES cells have the unique capacity to grow into any type of cell – brain cells, muscle cells, etc. Brivanlou is fascinated by the process that early embryonic cells use to make decisions about what kind of cell to become.
Brivanlou’s lab has used CRISPR/Cas9 (the DNA editing technology discussed yesterday) to induce the HD mutation in ES cells. So he can now compare, very precisely, the impact of the HD mutation on the developmental processes that he’s so interested in. Why do we care about this, don’t people with the HD mutation develop more or less normally? Yes – but we’d like to better understand what the huntingtin protein does. When we delete the HD gene in mice, they die before birth. So something the normal huntingtin protein does is critical for the developmental process from fertilized egg to healthy baby. Better understanding this role can only help us understand what goes wrong when the huntintin protein is mutated. Important reminder from Brivanlou, who says “a human is not a mouse”! Understanding human HD requires we study human cells. Brivanlou has found that mutating the HD gene causes specific changes in the signals that tell growing embryonic cells what to become.
Gerardo Morfini studies communication problems that occur in HD brains, before brain cells die they have problems ‘talking’. The main job of neurons, the cells that die most in HD brains, is to send signals to one another. These signals travel down long arms that scientists call ‘axons’, the part of the neuron Morfini is interested in studying in HD. Many brain diseases are caused by the early shrinkage, or retraction, of axons. When axons die, messages can’t be sent to other cells.
Morfini, and others, have observed that the mutant huntingtin protein slows down the trafficking of important stuff up and down axons. Axons can be long – the axon of your sciatic nerve begins low in your back and runs all the way to the tip of your foot! He’s discovered a change induced by mutant huntingtin protein that hurts the motors whose job it is to ferry stuff up and down axons. When he fixes this, HD mice get much better, suggesting he may be on to a new way to try to attack brain communication problems in HD. Morfini is now trying to identify drugs that might acheive the same benefits.
Many different types of neurons work together to make the brain function, forming in circuits that underlie behavior. Paola Arlotta wants to understand how each neuron in the brain decides which type of neuron it needs to be to make the circuits work. Her lab has developed techniques that let them disassemble intact brains and isolate each of the neurons that comprise the circuit. Normally, neurons decide which type of function they need to carry out during the early development of the brain, before we’re born.
She’s interested in the fascinating idea that we might be able to force neurons in the adult brain to become other types of neurons. She has shown that this is possible, allowing her to reprogram circuits in the adult brain in way not previously thought possible.
Ann Graybiel (MIT) is amongst one of the worlds foremost experts on a part of the brain called the basal ganglia. The basal ganglia are important for HD because they’re the most vulnerable part of the brain in the disease. The most obvious job of the basal ganglia is to help regulate movement – that’s why HD patients have distinctive movement problems. But scientists increasingly appreciate that these bits of the brain also play an important role in regulating moods and emotions.
Graybiel is interested in whether emotional problems in HD, like depression, might be due to dysfunction of the basal ganglia. Graybiel is studying these circuits in monkey brains, which are much more human like than mouse or fruit fly brain. They’ve identified very specific circuits that help the monkeys weigh cost/benefit decisions, which also involve basal ganglia. Graybiel is now making tools that will let her study how the circuits she’s identified are affected by the HD mutation.
Steve Goldman also studies the cells that comprise the brain, but he’s interested in a type a non-neuronal cells called glia. Glia were once thought to be the slightly uninteresting support cells of the brain, boring compared to their neuronal neighbors. But it’s become clear that glia have a huge range of important roles in the brain that importantly influence how the brain functions. One interesting thing about glia is that they, unlike neurons, continue to divide in the brain. Goldman’s lab has shown that a relatively small number of injected glia cells divide and end up populating the whole brain. He’s interested to understand whether changes in glial cells might contribute to how brain dysfunction in HD. His lab has developed a very interesting technique to create mice that have mouse neurons, but human glial cells!
By creating mice with human glial cells from HD patients, he can very precisely study how the HD mutation changes the HD brain. When mice have mutant HD genes in their glia, but not their neurons, Goldman finds that they have brain dysfunction like HD. This is surprising, and supports the idea that problems with glia could be part of HD in humans, as well. Goldman was interested if this would work the other way – he put normal human glia into HD mouse brains to see if this could help. HD mice look better and live longer when they have human glial cells, again supporting a potentially important role for glia in HD.
“Just because we can measure something doesn’t mean we can measure it well … and just because we can measure something well, doesn’t mean it’s important.”
“Just because we can measure something doesn’t mean we can measure it well … and just because we can measure something well, doesn’t mean it’s important.”
Thursday afternoon – measuring and modeling
This afternoon we’re looking at measuring and modeling Huntington’s disease – essential for running trials.
First up Doug Langbehn from University of Iowa. He is a stats whizz. He says: “Just because we can measure something doesn’t mean we can measure it well… and just because we can measure something well, doesn’t mean it’s important.” Langbehn did all the data analysis for the Track-HD study run by Sarah Tabrizi at UCL. Track-HD was the first major attempt to compare all our ways of assessing HD head-to-head: clinical, imaging, psychology tests & others. Langbehn puts a ton of thought into helping design studies and making sense of the results. We’ve got way better at this complex stuff. Things like participant dropout & missing data can screw up data analysis from studies. People like Doug work hard to make it work.
Next Tiago Mestre (University of Ottowa) reviews HD clinical rating tools – turning symptoms into numbers we can use to test drugs. You may be familiar with some of the rating scales – like the standardised neuro exam called the Unified HD rating scale (UHDRS). It’s crucial to understand how reliable scales are: what do they actually measure? How do they vary over time & between different raters? Mestre has undertaken a systematic review assessing and comparing all the rating scales used in HD. He found that HUNDREDS of different rating scales had been used, making it difficult to compare between studies. His team made evidence-based recommendations for what scales should be used for future studies and trials.
Jeffrey Long (University of Iowa) used data from huge HD studies (Track-HD, Predict-HD, COHORT, Registry) to assess various rating scales. Long’s intense analysis is producing better ways of predicting progression in HD and recruiting clinical trials.
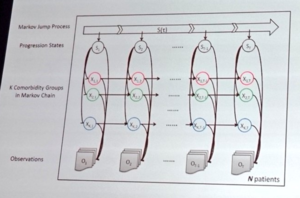
Jianying Hu from IBM’s Watson Lab has been bringing the awesome computing power of the Watson platform to crunching data in HD. Watson aims to take data from many sources and use “machine learning” to predict progression and help understand HD. If we’re lucky this will help guide treatment decisions and run clinical trials. Having built a computerised modeling system in lung disease, IBM Watson is now turning to HD.
And with that, the therapeutics conference comes to a thrilling conclusion!
But wait, there’s more! A surprise presentation from Dr. Rachel Harding, of the Structural Genomics Consortium with an exciting new effort. She’s interested in opening up the process of science – and has taken the very brave step of opening up her lab notebooks online. Anyone who wants to follow her experiments can catch up with what she’s doing every day at her website Lab Scribbles or follow @labscribbles on Twitter. It’s a brave adventure in “open science”.
